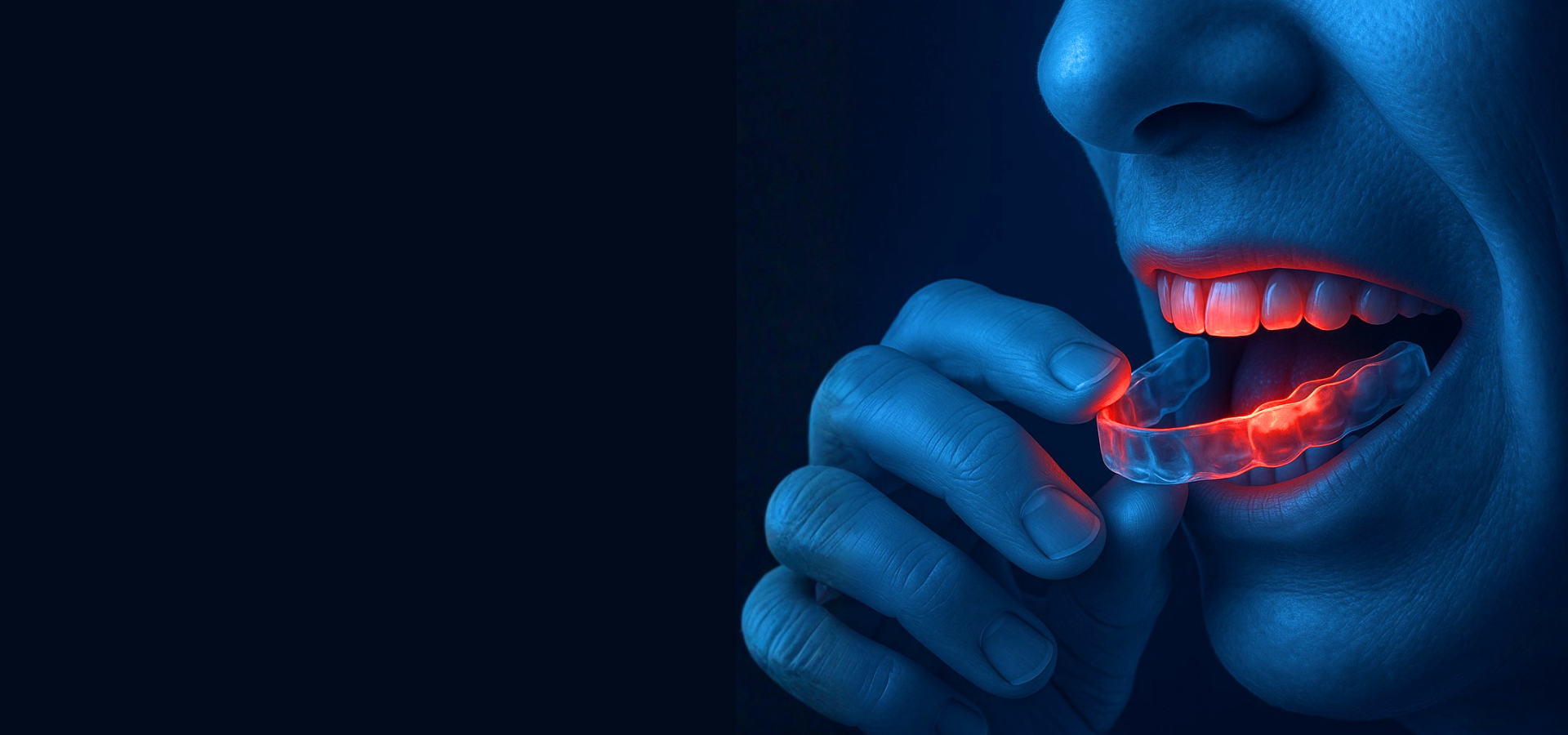
The Nightguard Mistake
Most Dentists Don’t Know They’re Making
Webinar for dentists - October 21, 2026
CE dental courses - Courses for dentists - TMJ Course
The Nightguard Mistake Most Dentists Don’t Know They’re Making
Course Overview
Nightguards and splints do not behave the same way in every patient. Many appliance complications begin long before the device is even fabricated. The real problem is not the guard. It is the system the guard enters.
When bruxism, clenching, or joint instability are not correctly identified, a nightguard can increase muscle activity, worsen joint strain, shift the bite, or accelerate instability. This webinar teaches dentists how to evaluate functional patterns with clarity, how to choose the right appliance, and how to design orthotics that support the joint rather than overload it.
You will learn how different appliances influence muscle behavior, occlusal loading, and joint stability. Real clinical cases show why some guards succeed, why others fail, and how the right diagnostic steps make outcomes predictable and stable.
What You’ll Learn:
1. How do I differentiate bruxism from clenching and why does it matter for appliance selection
Identify clinical signs, history patterns, and muscle behaviors that distinguish grinding from clenching so the correct appliance type is chosen for the correct functional pattern.
2. How do I know which nightguard or orthotic is appropriate for each patient
Match appliance design to functional patterns such as bruxing, clenching, parafunction, or suspected TMJ instability using a predictable decision sequence.
3. How do different appliance designs affect muscles, joints, and occlusion
Explain how variations in guidance, vertical dimension, and occlusal contact on appliances influence muscle recruitment, joint loading, and bite stability.
4. How can I tell if a nightguard is making symptoms worse instead of better
Recognize early red flags such as bite shifting, muscle tenderness, joint clicking, morning headaches, and loss of stability that signal an appliance was not correctly selected.
5. What steps should I complete before recommending a nightguard or splint
Perform a structured TMJ and occlusal evaluation that includes joint assessment, muscle palpation, functional movement analysis, and risk screening to ensure the appliance will not worsen instability.
6. How do I adjust, refine, or redesign appliances to support TMJ stability
Apply practical strategies to modify contact intensity, guidance patterns, vertical dimension, and occlusal balance so the appliance decreases functional strain and improves clinical outcomes.
Date: October 21, 2025
Time: 8:00PM EST
Format: Webinar
Cost: Free
CE Credit: 1
Presenter: Dr. Agatha Bis
INSTRUCTOR QUALIFICATIONS:
Dr. Agatha Bis has over 30 years of clinical experience with a special focus on TMJ & TMD management.
Known for her expertise in both, diagnosis and treatment, Dr. Bis is a leader in TMD education and dedicated to improving patient outcomes through advanced knowledge and skills.

